When Leah Cerwinske and her husband were expecting their first child, she was the picture of health. As a fit and active 30-year-old dietitian, she had the knowledge, habits and motivation to enjoy a healthy pregnancy. After an uncomplicated pregnancy, she delivered a baby girl. But then, Leah’s blood pressure soared unexpectedly. Even without a history of high blood pressure, she developed post-partum pre-eclampsia, a serious condition that can be life-threatening.
“It was a surprise,” Leah said. “I eat well, and I avoid processed food and high sodium, even more so when I’m pregnant, and I gained only as much weight as I was supposed to gain.”
Now four years later, Leah, her husband, Luis, and their daughter, Madeline, are celebrating her fourth Mother’s Day — and preparing for the birth of their newest member of the family.
Beyond the immense demands of motherhood, women who’ve carried and delivered a baby put their bodies through enormous physical changes that can challenge their heart and vascular systems.
Leah’s body was responding to the demands of pregnancy, which nearly doubles the volume of blood in a woman’s body. To circulate all that blood, the heart must pump faster and work harder, said cardiologist Rupa Sanghani, MD, director of the Rush Heart Center for Women.
“Pregnancy is like a nine-month-long stress test,” she said. “It can unmask heart problems or provide clues to what conditions may arise in the future.”
With the body working extra hard to circulate blood and nourish the fetus, a woman may develop “gestational” high blood pressure, diabetes and pre-eclampsia, which can cause complications such as early (preterm) labor. Gestational conditions occur during pregnancy or in the days after delivery and usually are temporary.
Pre-eclampsia, which means “before a seizure,” involves more than high blood pressure. The condition is marked by very high blood pressure and protein in the urine — a sign that the kidneys are stressed. Other symptoms are severe headache and/or very swollen legs or feet, what’s called “edema.”
“The big concern with pre-eclampsia is that the mom can progress to having a seizure, which puts her and her fetus in danger,” Sanghani said. “Pre-eclampsia also signals to us that the mother’s blood vessels and vasculature are not normal, that they are limiting blood flow to the baby.”
Having gestational hypertension or pre-eclampsia affects not only this pregnancy but also increases the likelihood of having these issues in future pregnancies.
“It also leads to higher cardiovascular risks for the mom later on in life.” she said.
Many develop chronic high blood pressure within 10 years of their pregnancy. The same vascular issues that may lead to pre-eclampsia can be related to the risk of future heart disease, she said.
Known risk factors
Women are at greater risk of developing gestational conditions if they are obese, over age 35, have or have had high blood pressure, a heart problem or inflammatory disease, or if they had complications in an earlier pregnancy.
“But women who don’t have any known risk factors can develop high blood pressure or pre-eclampsia, too,” Sanghani added.
Leah can attest to that. She had a smooth pregnancy with the usual ups and downs. After delivery, on the day she and her husband were to go home with their baby, she woke up feeling poorly and with a tightness in her chest. Her nurse checked her blood pressure and, for the first time, it was very high. Leah was diagnosed with gestational hypertension. With directions to monitor her blood pressure, she and her baby checked out.
On the drive home, though, “I just didn’t feel myself,” she said. Once at home, her chest hurt again, and she felt light-headed. Her blood pressure again was extremely high. Returning to the hospital, she was readmitted, and after a series of tests, she was diagnosed with post-partum pre-eclampsia.
“I didn’t even know you could develop this after delivery,” Leah said.
After two days of care in the hospital, Leah returned home, followed up with her doctors and had no additional complications.
‘It can happen to anyone’
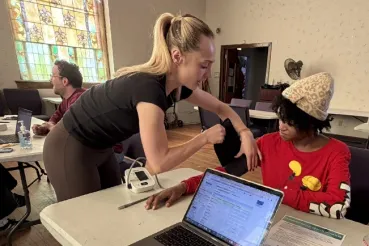
Throughout her current pregnancy, Leah has been vigilant in watching her blood pressure and following up with Sanghani. And, so far, so good. She continues to exercise, eat nutritiously and check her blood pressure weekly.
“Even if I do all the right things to prevent it, I could still develop hypertension now or chronic hypertension in the future,” she said. “It can happen to anyone.”
She’s using her awareness to stay in tune with how she feels, which will be just as important or more so in the first days, weeks and months after baby arrives.
The ‘fourth’ trimester
In the weeks after giving birth, the body faces additional demands that may cause problems for some women, especially those who’ve had blood pressure or cardiovascular concerns, Sanghani said.
“After delivery, your blood vessels clamp down significantly. Yet you haven't had a chance to release all the excess fluid from your body,” Sanghani said. For anyone who had problems with high blood pressure or any condition in which the heart is not squeezing well, “this creates a very vulnerable situation.”
The heart is a muscle, and during pregnancy it’s used to a relaxed, regular load. Then suddenly, the muscles around the blood vessels constrict, making it harder for the heart to pump blood through the body, and the heart struggles.
“It's like lifting weights,” she said. “Lifting a two-pound weight is manageable, but suddenly lifting a 20-pound weight can cause the muscle to give out.”
The other postpartum concern is universal: “You are all caught up with the new baby and not thinking about yourself,” she said. “But you are exhausted. You're recovering from a major physical event, you're sleep deprived.”
She asks her patients to check their blood pressure every day for the first two weeks, and to see her (sometimes via telemedicine) the first four to seven days.
The term “fourth trimester” describes the postpartum time when mothers are still recovering and adjusting. It’s also the time when pregnancy-related death or illness can occur. In fact, most maternal deaths occur after delivery.
“New moms can't forget about themselves, and they need to let other people help out with the baby,” she said. “No. 1: They need to be aware that they are at risk.”
What to watch for and what to do
Pregnancy is full of symptoms: You get short of breath, tired, feel nauseated. “Those are all normal parts of pregnancy,” Sanghani said. So when do you need to take action?
If a symptom is getting worse gradually, like you are getting more and more short of breath with the pregnancy, that is usually fine, she said. “If all of a sudden, though, like in a day or two, you are really winded, more than you have been, that’s when you need to let your doctor know.”
Even so, Sanghani said it’s best to call your obstetrician or cardiologist, if you have one, with any concern, even if it might not turn out to be a problem.