Rush University Medical Center is the first in Chicago and one of the first in the nation to offer a new FDA-approved telemedicine option for deep brain stimulation patients. Using the new system by Abbott called NeuroSphere Virtual Clinic, patients and their physicians are now not only able to communicate remotely, in real time, but also to prescribe treatment settings and ensure a proper response and device functionality.
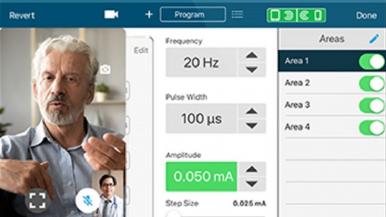
Through NeuroSphere Virtual Clinic, the physician and patient connect via a secure in-app video chat. The remote programming feature, available within the Abbott patient controller app, provides a simple and secure connection during which the clinician can prescribe treatment settings remotely to the patient's neurostimulation device.
Rush was chosen as one of only a handful of medical centers to help launch the remote neuromodulation technology, which is the first of its kind in the United States.
In deep brain stimulation treatment, electrodes implanted in targeted areas within the brain provide electrical pulses to help control symptoms such as tremors — similar to the way a heart pacemaker works. The electrodes are connected to the neurostimulator, a small device implanted under the skin below the collarbone.
Deep brain stimulation, or DBS, is used to treat movement disorders such as Parkinson's disease and essential tremor. “Although not a cure, DBS can be a life-changing experience for appropriate PD and ET patients, patients,” says Leonard Verhagen, MD, PhD, director of the Movement Disorder Interventional Program at Rush University Medical Center. “DBS can help patients regain the ability to sign their name legibly, feed themselves and perform other activities of daily living.”
A DBS system requires a series of clinic trips to prepare for, implant and begin neurostimulation. Once the stimulation is started, it can take several appointments to find the setting that optimally improves symptoms. Additionally, patients may need two or three adjustments to the settings each year. With Abbott’s NeuroSphere Virtual Clinic, patients are offered the flexibility and comfort of receiving these adjustments and follow-up care from anywhere. Remote programming, with NeuroSphere Virtual Clinic, may be performed in any location where the patient has a cellular or Wi-Fi connection and a sufficiently charged patient controller.
“This will be a great convenience for our DBS patients with movement disorders who have a long distance to travel or who have difficulty leaving the house because of their condition,” Verhagen says. “Sometimes, patients need to be off their medication for a period of time before the DBS settings are adjusted, which adds another hurdle to making an office visit.”
“Telemedicine is increasingly recognized as an efficient care model that is the way of the future, and remote programming ensures that our patients with DBS systems are not left behind.”
Rush University Medical Center has Centers of Excellence and Centers of Care for Parkinson's disease and other movement disorders. Rush provides the most deep brain stimulation treatment in the Chicago metro area. Patients come to Rush for DBS from Downstate Illinois, Wisconsin, Iowa, Indiana and other places hundreds of miles from Chicago.
NeuroSphere Virtual Clinic is compatible with Abbott's suite of neuromodulation technologies, including Infinity DBS System for patients with Parkinson's disease and tremors of the upper extremities in adults with essential tremors; Proclaim XR SCS System for patients living with chronic pain of the trunk and/or limbs; and Proclaim DRG Neurostimulation System for patients with chronic pain in the lower limbs caused by complex regional pain syndrome or causalgia.