When 82-year-old Antti Talvitie, PhD, learned he needed surgery to treat a blood clot in his brain, he was stunned to hear he’d likely go home the same day with just a small bandage on his wrist. Thanks to a clinical trial at Rush, Antti had a minimally invasive procedure that helped him return quickly to his active retirement.
Unsettling symptoms
A couple years ago, Antti noticed something unusual while he was playing pickleball. When he picked up the ball, its texture felt strange in his left hand — but totally normal in his right.
At first, he brushed it off. Soon, though, he realized his left hand wasn’t working quite right. Shaving became tricky, using a fork and knife was difficult and other everyday tasks felt clumsy. So he decided to mention these episodes to his primary care physician, Jill Marcus, MD, during his annual physical.
Although Antti’s symptoms weren’t debilitating, they were unnerving. And Marcus took them seriously.
She explained that issues like this could be caused by a blood clot or mini stroke that blocks blood flow to the brain.
She ordered a brain CT scan to get a clearer picture of what was going on. Antti’s scan revealed a subdural hematoma, a blood clot pressing on his brain, likely caused by a minor fall or head bump several weeks or months earlier.
Marcus promptly referred Antti to neurosurgeon R. Webster Crowley, MD, who specializes in treating this type of hematoma.
“With a subdural hematoma, you might have a little bit of a bleed that expands over time, especially as you get older,” Crowley explains. “As these small bleeds leak more or evolve, they can swell and cause symptoms.”
A new approach to brain bleeds
At Antti’s first appointment, Crowley educated him about subdural hematomas and how it was causing his disconcerting symptoms.
He then shared several ways they could treat it, including:
- Watching and waiting to see if his symptoms worsen
- Open brain surgery to remove the clot
- Embolization to cut off the blood supply to the clot
- A combination of surgical removal and embolization
One of the biggest challenges with subdural hematomas is that even with surgical removal, they often come back (known as recurrence) and frequently require additional surgeries. One of the reasons for this is the blood supply that these hematomas may develop, essentially keep them alive and allow them to grow and press further onto the brain.
Crowley explains that these blood clots typically have a robust blood supply that comes from the middle meningeal artery, an artery in the covering of the brain. These arteries can cause repeated bleeds, even when surgery to remove the hematoma is successful.
That’s where the clinical trial at Rush came in. Crowley told Antti about an innovative procedure called middle meningeal artery embolization (MMA). Crowley has been performing MMA embolization for years for other conditions like brain tumors and dural arteriovenous fistulas. But new data suggested MMA embolization could also be beneficial for subdural hematomas, which led to the clinical trial.
Trial investigators suspected that cutting off the blood supply to the covering of the brain and the membranes of the clot, would decrease the need for additional surgeries.
After learning about the trial, Antti was intrigued. “I wanted to participate in the trial because I wouldn’t have to wait and see if my symptoms got worse; I could take care of it right away,” he says. “I’m also a scientist by training, and I trusted the medical professionals. I felt very comfortable with the plan.”
A minimally invasive brain procedure
Instead of open brain surgery, the MMA embolization is a minimally invasive procedure. Crowley and his team went through a very small needle puncture in Antti’s arm, and used catheters (small, flexible tubes) to access Antti’s brain.
“It’s a very common technique, often used for imaging blood vessels throughout the body, or for treatments such as placing stents anywhere from the legs to the brain, as well as the heart,” Crowley says. “In this case, we went through an artery in his wrist and carefully snaked our way to the middle meningeal artery.”
Crowley then embolized the MMA by injecting a glue-like material into the artery to cut off the blood supply to the blood clot. After he completed the embolization, Crowley removed the catheter and placed a bandage on Antti ’s wrist.
“Basically, he had a little needle puncture similar to an IV and a little bandage on his wrist, which definitely beats a hole in your head,” Crowley says.
Lower risk, fewer recurrences
One of the biggest advantages of MMA embolization is it’s less risky than open surgery, especially for older adults.
“You can have the embolization and still go on to need surgery, but it dramatically decreases the chance of needing that surgery,” Crowley says. “As a brain surgeon, I am hopeful that we can decrease the number of people who need brain surgery.”
Initially the procedure was considered a good option for people who were not ideal candidates for brain surgery, such as older patients, or those in poor health who may not be able to tolerate general anesthesia or open-skull surgery.
However, the results of the trial made it clear the procedure may potentially benefit almost anyone with a subdural hematoma.
The clinical trial ultimately found that MMA embolization reduces recurrence and the need for additional, more invasive surgeries. In fact, when results were published in the New England Journal of Medicine, the study authors, including Crowley, concluded MMA embolization should now be considered standard of care for many subdural hematomas.
Today, surgeons now perform this as a stand-alone treatment for people who have mild symptoms, helping to prevent enlargement of the hematoma and the need for an open brain surgery. For people who have larger hematomas or more severe symptoms, surgeons can perform an MMA embolization in conjunction with surgery to decrease the chance of needing more procedures in the future.
With an aging population, Crowley is, in fact, seeing more people who have subdural hematomas. And having an alternative for those who would like to avoid open brain surgeries allows him and his colleagues to offer potentially safer treatment to their patients.
“For these patients, we may be able to get rid of the blood clot by doing an MMA embolization, which we can also do awake (rather than with general anesthesia),” Crowley says. “Or for those who needed the open surgery, we can decrease the chances that they would have a recurrence and need more open brain surgeries. It’s a lower risk procedure than an open brain surgery and has allowed us to treat more people safely and effectively.”
Back to living life
After his MMA procedure, Antti’s symptoms disappeared almost immediately. He had regular follow-ups, including regular CT scans. After a year of follow-ups, Antti no longer needed monitoring — and he’s been symptom-free since.
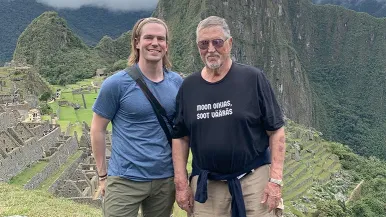
Today, two years after his treatment, he’s back to enjoying a full and active life, playing pickleball, traveling and spending quality time with friends and family.
“I’m back to normal, just like I was before I had the hematoma,” he says. “I feel very good about it, and I am quite satisfied with the treatment and care from Dr. Crowley and his team; there was a whole team supporting me and it went so smoothly.”