More than 50 years since the first White House Conference on Hunger, Nutrition and Health in 1969, thousands of studies have made the same conclusion: A coordinated strategy to end hunger, improve nutrition and physical activity and close the disparities surrounding these issues is essential for ending health inequity.
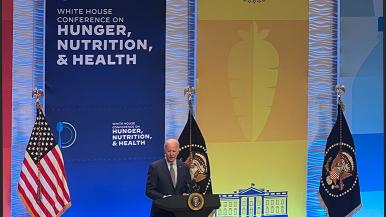
When the conference reconvened on Sept. 28 in Washington, D.C., Rush experts were at the table to pledge support and to demonstrate the effectiveness of its strategy to address these issues.
For decades, Rush University System for Health has demonstrated its deep commitment to addressing inequities in health care, and health equity has evolved as an internal and external strategy at Rush since 2016. Specifically, Rush strives to measurably reduce inequities across our patients, learners, people, communities and organization — an effort complementary to that of the White House Conference.
“The return of the White House Conference on Hunger, Nutrition and Health is a welcome affirmation of the importance of this work,” said Anil Saldanha, Rush chief innovation officer. “Its goal of ‘catalyzing the public and private sectors around a coordinated strategy to end hunger, improve nutrition and physical activity, and close the disparities surrounding these issues’ aligns perfectly with the Rush work in this space.”
Reducing life expectancy gap
Specifically, Rush — through the RUSH BMO Institute for Health Equity and West Side United — is working to reduce the life expectancy gap by 50% by 2030. Research demonstrates that during a ride west on Chicago’s El, one will see a 12-year drop in life expectancy between the Loop and West Garfield Park.
“The phrase ‘food is medicine,’ captures it perfectly,” said Saldanha. “As health care organizations, we must treat the entire patient, and recognizing the reality of food insecurity and the impact it can have on a patient’s post-hospitalization must be woven into discharge processes. At Rush we are working to formalize questions relating to food and nutrition into the patient experience.”
Rush is piloting new technology via our Cancer Center to connect patients with resources and make interventions before a risk becomes a reality.
“Understanding the conditions that patients are returning to as they continue to recover is essential to ensuring they are on the road to healing,” said John Rich, MD, MPH, director of the RUSH BMO Institute for Health Equity. “Additionally, asking these key questions reminds clinicians of the importance of understanding how health-related social needs and social determinants of health are a significant part of the care equation of each unique patient.”
By piloting new technology to address the issue as part of the patient experience now, Rush is well-positioned to meet requirements being phased in by the Centers for Medicare and Medicaid Services. The first-ever set of measures of social determinants of health was adopted by CMS in August and will become mandatory in 2024.
Rush committed to the White House call to action as a part of Sync for Social Needs, a coalition working to unite leading health technology companies and health systems to standardize the sharing of patient data on social determinants of health, including food insecurity.