Mentor Program Fosters Role Consistency, Quality
The emergency department’s (ED) primary function is to treat critically ill and severely injured patients. Well-designed triage systems with knowledgeable, skilled, empowered triage nurses (RNs) are central to reducing patient morbidity and mortality, improving patient satisfaction and increasing the efficiency and effectiveness of ED services. The specialized function of this RN triage role is unique to the ED. Although all clinical nurses perform assessments, the triage RN — supported by the Illinois Nurse Practice Act and Emergency Nursing Association (ENA) standards of practice — performs complex assessments and makes independent decisions based on the full scope of nursing practice.
Triage is a dynamic process that requires skilled nursing assessments and decision-making. Rush University Medical Center adopted the ENA practice standards and position statement, which outline role qualifications and advanced skills for prioritizing patients based on physical, psychological and social needs and factors influencing flow through the emergency care system. Some RN qualifications include a minimum of one year of emergency room experience, completion of triage-specific education, and ongoing triage competency validation.
The nationally recognized, evidence-based five-level Emergency Severity Index (ESI) helps to guide the triage nurses’ critical thinking. The ESI prioritizes patients based on the urgency of their condition to receive medical care. The detailed ESI includes questions considering the patient’s acuity, including “When should the patient be seen?” and resources, such as “What does the patient need?”
Emergency Severity Index (ESI)
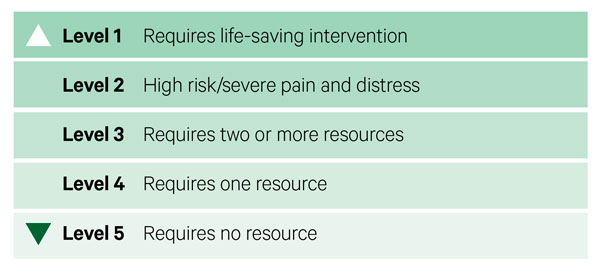
Level one is the most acute, and level five is the least urgent. More specifically, levels one and two are based on patient acuity, and levels three through five focus on resource needs. The goal of applying this index scale is to standardize decision-making and connect every patient to the right resources in the right amount of time.
To make effective and safe triage decisions, nurses must draw from extensive knowledge and experience to act based on the patient’s presentation. Since the triage RN functions autonomously, it is vital to ensure a standardized orientation supports role development and ESI application, which guides patient prioritization consistency. Foundational triage nurse training includes the following:
- Completion of online triage modules
- Attendance at four triage workshops led by the unit clinical nurse specialist
- Attendance at a minimum of 16 clinical triage orientation hours with a preceptor
A workgroup was formed in July 2023 to foster ongoing critical thinking development that supports role consistency and quality. The team was led by Sara Henry, BSN, RN, CEN, interim assistant unit director; Ashley Boumgarden, DNP-FNP, BS, RN, clinical nurse RN3; and Marites Gonzaga-Reardon, DNP, APRN, CCNS, CEN, Clinical Nurse Specialist and the mentor program team includes Peyton McDade, BSN, RN, Nancy Berger, RN, Hannah Vaughan, BSN, RN, Kellie Tuley, MSN, CNL, CMSRN, and Alicia Taylor, BSN, RN.
Following triage nurse training, new triage nurses are assigned to an experienced triage RN mentor. The mentor program received positive feedback from new triage nurses, mentors and interdisciplinary team members. Ensuring thorough triage role training via this mentorship model supports role consistency and the delivery of quality patient care.