Background
- Prompt treatment of patients presenting with suspected ischemic stroke remains a priority for emergency departments globally.
- Timely intervention is dependent on a well-functioning team and efficient processes.
- Due to the urgent nature of a Code Stroke, effective communication, streamlined workflows, and role definition are crucial for making sure patients can be treated efficiently.
- An urban academic comprehensive stroke center’s stroke performance improvement committee noted a trend of increasing door-to-needle (DTN) times overall, achieving the center's goal of DTN <60 minutes only 60% of the time. This did not align with the American Heart Association (AHA)’s Target: Stroke Phase III goal of treating 85% or more patients within 60 minutes.
- The urgent need to reduce times, as well as the multifactorial nature of delays, required a creative approach to address several opportunities at once.
Purpose
Implementation of a bundle with a goal of reducing DTN times and improving interdisciplinary communication and collaboration at a single comprehensive stroke center.
Methods
- The intervention was done at a single, academic, comprehensive stroke center.
- A multidisciplinary stakeholder group formed to develop an action plan.
- Due to the urgent need to address the issue, several initiatives were introduced simultaneously as a bundled approach. All interventions were at no cost to the institution. The bundle included the following:
- Interdisciplinary stroke huddle
- Clock
- BP monitor/IV starts in CT
- EMS registration
- Streamlining orders
- Unit-based stroke committee
- Increased communication, transparency, recognition to ED staff
- Data was compared 14 months pre-implementation of the bundle to 14 months post-implementation during 2022-2024.
- All patients that received Tenecteplase (TNK) in the ED were included, regardless of final diagnosis. However, if patients met valid exclusion criteria for time-based goals according to the AHA Get With the Guidelines® database (i.e. management of concomitant emergency situations), they were excluded.
Results
| Table 1. Pre- and Post-Intervention Comparison | ||
|---|---|---|
| Pre-Intervention | Post-Intervention | |
| Number of Patients, n | 35 | 49 |
| Mean DTN (minutes) | 55 | 45 |
| Median DTN (minutes) | 59 | 46 |
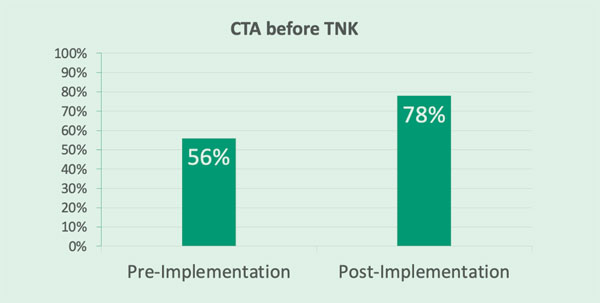
| CTA before TNK | 56% | 78% |
Figure 1. DTN Times
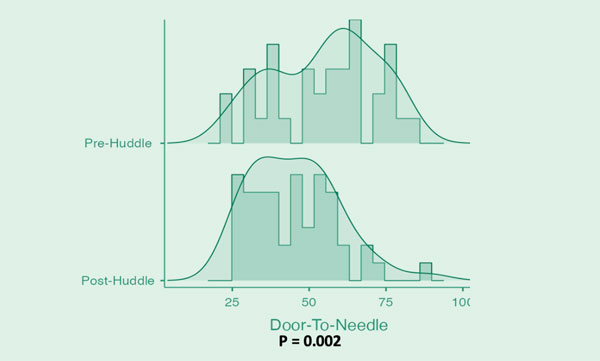
Figure 2. Treatment Goal Adherence
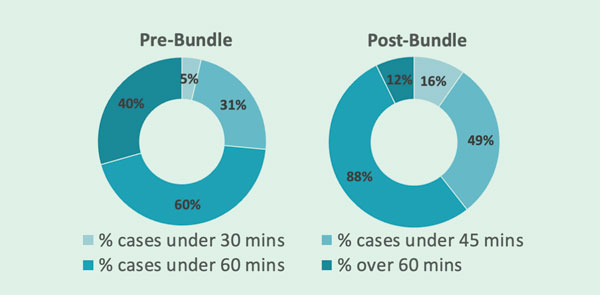
Figure 3. CTA Pre-TNK
Discussion
Post-implementation of bundle, there was an 18% decrease in mean DTN times. There was also a significant shift in performance for each Target: Stroke Phase III goal. The medical center met the goal of DTN <60 mins for 85% of patients for CY24. Notably, this post-implementation reduction in door to needle times was achieved while simultaneously obtaining CTA before TNK in a higher percentage of patients, allowing for expedition of thrombectomy for large vessel occlusion strokes while simultaneously optimizing door to needle times for patients eligible for thrombolytic therapy.
Conclusion
After implementation of the bundle, DTN times were significantly reduced, and communication has been much improved. Staff feedback has been positive, and all components of the bundle are sustainable. The medical center continues to reevaluate and refine this process.