Fiscal year 2024 was another successful year for the Rush Department of Professional Nursing Practice (PNP). The department continued to achieve its mission of promoting the highest quality of care at Rush University Medical Center through professional development, interprofessional collaboration, innovation, and expertise in data, evidence-based practice and quality improvement. The following programs and projects highlight how the department continues to achieve its mission and surpass its goals.
Single Center Outcomes of Hospital-Acquired Pressure Injury Disparities (HAPI-D) Before, During, and After COVID-19
- Lisa Boudreau, MSN, RN, CWOCN
- Andrea Deja Fidai, MSN, RN, CWON, CNL, CMSRN
- Mary Ellsworth, MSN, RN, CPHQ, NPD-BC
- Michele Sanford, BSN, RN
- Mary Heitschmidt, PhD, APRN, CCRN, FAHA
- Robert J. McCarthy, PharmD
A retrospective research study was conducted at the medical center to examine the self-reported race and ethnicity of patients with hospital-acquired pressure injuries before, during and after COVID-19. It has been shown that higher rates of hospital-acquired pressure injuries are noted in Black, Hispanic and Asian patients compared to Caucasians in hospital and long-term care facilities. However, acute care descriptive studies evaluating pressure injuries in Black, Hispanic, and Asian patients with COVID-19 are lacking.
This project was a collaboration between the wound ostomy nurses, data analysts, the director of clinical research for the Professional Nursing Practice, and the director of anesthesia research. Results found distribution differences in the severity and number of pressure injuries in COVID-19 patients compared to non-COVID-19 admissions. COVID-19 patients were also more likely to be Hispanic, have Medicaid or be uninsured, have diabetes, and be on corticosteroids, vasopressors and mechanical ventilation. Additional research is needed to improve pressure injury risk assessments that include conditions related to the social determinants of health and the severity of illness.
A research poster was presented at the National Wound Ostomy Continence Nurse Society Conference in Cleveland, Ohio, in June 2024. The abstract was published in the evidence-based and peer-reviewed Journal of Wound, Ostomy, and Continence Nursing (JWOCN®).
Diabetes Clinical Support Team
- Emily Brey, MSN, APRN, AGCNS-BC, CDCES
- Bernadine Holland, MSN, MBA, RN, BC-ADM, CDCES
The Diabetes Clinical Support Team (DCST) is a nurse-driven initiative designed to enhance the care of patients with diabetes by providing members with comprehensive knowledge and skills through education. The training includes but is not limited to:
- Advanced pathophysiology of diabetes
- Information on the latest medications and technology
- Application of inpatient policies and protocols
The DCST nurse is a resource to colleagues and a catalyst in improving care and safety for patients with diabetes. Examples regarding care and safety improvements include the following:
- Identifying risks for hypoglycemic events or gaps in patients with diabetes
- Self-management and steering to the appropriate resources
- Support professional growth and movement up the clinical ladder
The DCST quality improvement project is being piloted on a general medicine floor (9 Kellogg) and observation unit (5 Kellogg) and will eventually expand to other inpatient units.
Developing Talent in Rush Anchor Mission Communities
- Pheonix Silverlight, MSN, RN, CNL
- Hadley Landeryou, MSN, RN
- Angela Geschrey, MSN, RN, CMSRN, NE-BC
- Jacqueline Cwiok, MSN, APN, AGNP, FNP-BC, LSSGB
- Brent Alwood, MSN, RN, CNML
Patient care technicians (PCTs) support nursing and provider practices with skills in patient monitoring. The PCT Apprentice Program was developed to reduce barriers to entry into healthcare careers for members of the Rush anchor mission communities. Launched consecutively at Rush University Medical Center and Rush Oak Park Hospital during fiscal year 2024, the program provides individuals with no prior healthcare experience or knowledge an opportunity to train as a Certified Nursing Assistant (CNA), a requirement to become a PCT.
This grant-funded program gave participants four weeks of CNA training and one week of professional development coaching. Participants were hired as full-time, benefitted employees throughout their training to reduce financial barriers that might otherwise have inhibited their success in training. After passing their CNA certification exam, they were guaranteed interviews at Rush and were hired to work on units as PCTs.
This group was encouraged to “dream big” and was supported in considering their next steps. Many apprentices have shown interest in becoming nurses, some are interested in being a radiology or surgical technician, and others want to perform phlebotomy.
As the program continues to develop, PNP plans to assist these individuals in expanding their interests and pursuing education as appropriate. During fiscal year 2024, PNP supported eighteen PCT apprentices in transitioning into the PCT role on numerous units throughout the medical center. The team was thrilled to identify that retention rates for PCT apprentices were about 20% higher than when compared to PCTs hired outside of this program.
Life-Saving Hands – Training Our Neighbors
- Brent Alwood, MSN, RN, CNML
- James Haukland, BS, EMT-P, CHSE, CHSOS
- Michelle Czmil, BA
- Miriam Ramirez, MSN, RN, CEN
- Saraly San Pedro, MSN, RN, NPD-BC, CRRN
The Professional Nursing Practice department and Training Center wanted to align with Rush’s anchor mission to decrease healthcare disparities in our local urban community by addressing the need to improve responsiveness and gaining skills to manage emergencies.
Training Our Neighbors is a program that provides AHA Heartsaver® certification to West Side community members at no cost to the participants. The training includes a review of cardiopulmonary resuscitation, choking, use of an automatic external defibrillator and first aid training. This program aims to increase the participant's knowledge, skills and confidence when intervening during pediatric and adult emergencies and to reduce morbidity and mortality throughout the West Side of Chicago communities.
During fiscal year 2024, the program worked with community partners, including churches, schools and community centers. It trained 210 West Side community members and increased their knowledge, skills, and confidence in responding to emergencies.
Pre-Assessment/Before Class
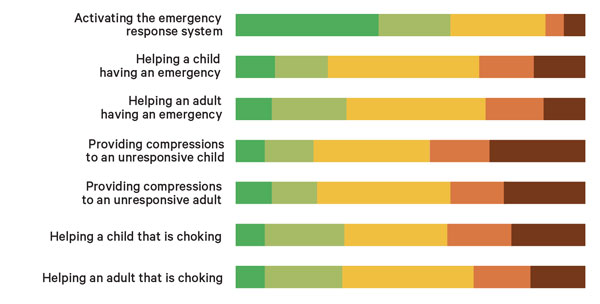
Post-Assessment/After Class
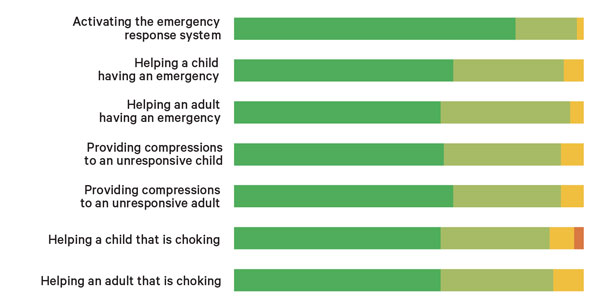
Key

By the Numbers
| Wound Ostomy Continence Nurses | |
|---|---|
| Patient encounters | 3,715 |
| Hours delivering staff education | 153 |
| The HAPI prevalence rate of 0.43% exceeded the goal of 0.59%. | |
| Diabetes Clinical Nurse Consultant | |
|---|---|
| Patient encounters per month | 309 |
| Direct Patient care min per month | 6785 |
| Vizient® - Severe hypoglycemia rate | 3.15% |
| Nursing and Assistive Personnel System Orientation (NAPSO) Attendance | |
|---|---|
| Total attendees | 1200 |
| RNs | 685 |
| Assistive Personnel | 515 |
| Participation in PNP Workshops | |
|---|---|
| Improvement Lab | 101 |
| Nursing Preceptor Class | 252 |
| Charge Nurse Class | 185 |
| Training Center Numbers: 5,011 | |
|---|---|
| BLS | 2957 |
| ACLS | 1354 |
| PALS | 434 |
| Heart Saver | 366 |