RUSH neurosurgeons have integrated the ExcelsiusGPS (Excelsius) robot into their neurosurgical treatment options. Rush’s neurology and neurosurgery program is ranked No. 4 in the country, and its practitioners are employing Excelsius as part of its range of the latest minimally invasive techniques for corrective spinal procedures, such as spinal fusion, adult deformities and scoliosis correction.
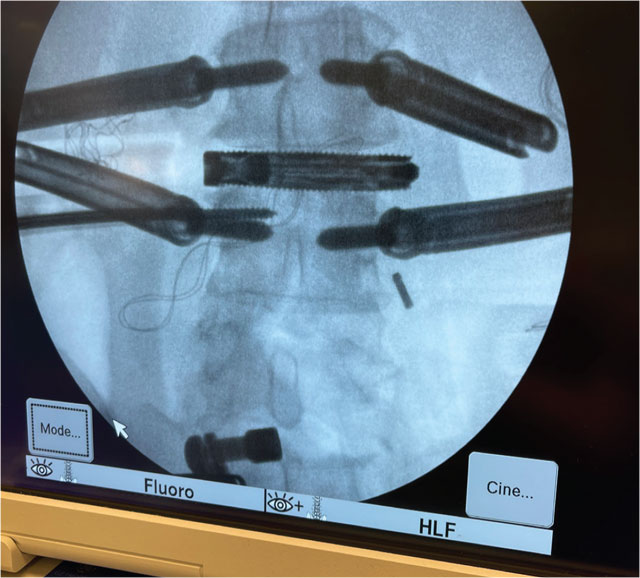
The robot has improved the accuracy and replicability of implant and pedicle screw placement in corrective spinal surgeries through image-guided navigation while also reducing the radiation exposure of patients and operating room personnel. Additionally, Excelsius has been used in some cases to shorten the length of incisions needed to access the spine, which ultimately can reduce the length of stay.
The following are three types of cases that highlight the advantages Excelsius provides RUSH neurosurgeons.
Adult deformity correction
Minimally invasive surgery, such as anterior lumbar, direct lateral and oblique lateral interbody fusions, is the preferred approach when feasible in the treatment of adult spinal deformities such as scoliosis and kyphosis. Depending on the type of fusion being performed, surgeons may utilize metal plates, rods and screws, with the overall goal being to reduce the curvature in the affected areas of the spine and prevent further progression of the condition.
The benefits that Excelsius provides
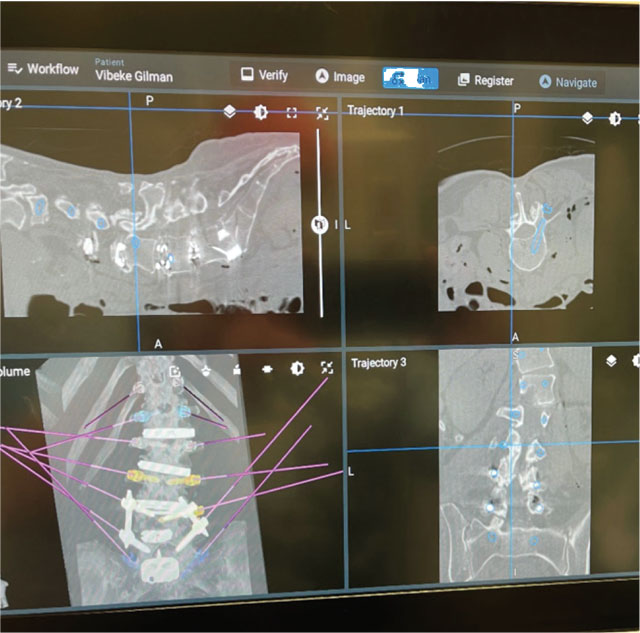
Depending on the severity of the patient’s condition, the Excelsius robot can enhance these minimally invasive approaches with preoperative and intraoperative imaging through its robotic arm. As with pediatric scoliosis cases, this imaging helps to ensure greater precision for implant and screw placement.
As neurosurgeons pull or shift bone or apply pressure that changes the curvature of the spine, proper fixation of the implant and screws is paramount to avoid pullout, especially for patients who need larger and longer implants to correct their deformity.
Robotic Adult Deformity Correction
Robotic MIS Lumbar Deformity: Stage 1
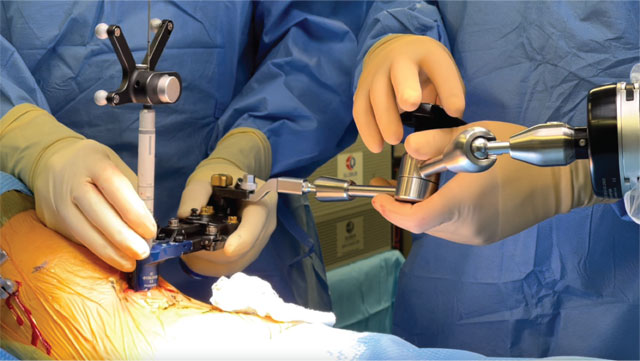
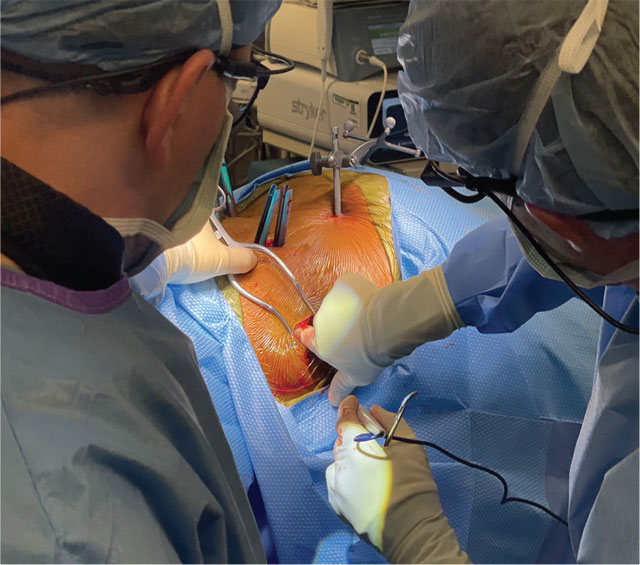
Intraoperative photographs showing the use of the robotic 3D navigation instruments to perform lateral lumbar fusion and deformity correction under endoscopic visualization.


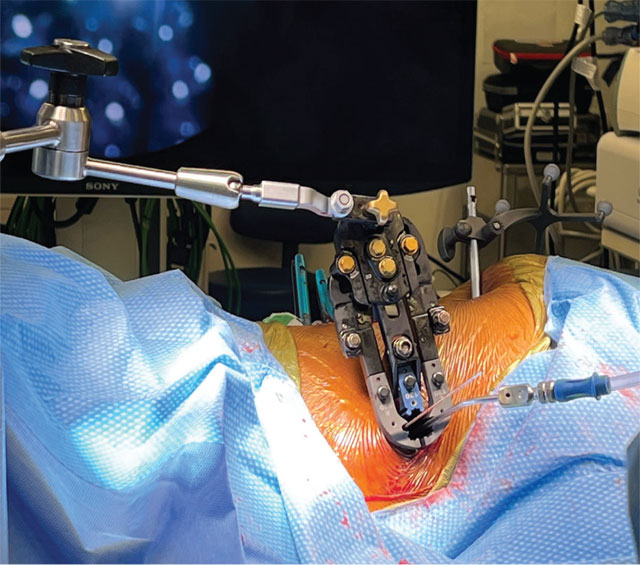
Intraoperative photographs showing the use of the robotic 3D navigation system to plan and place posterior spinal instrumentation for deformity correction.

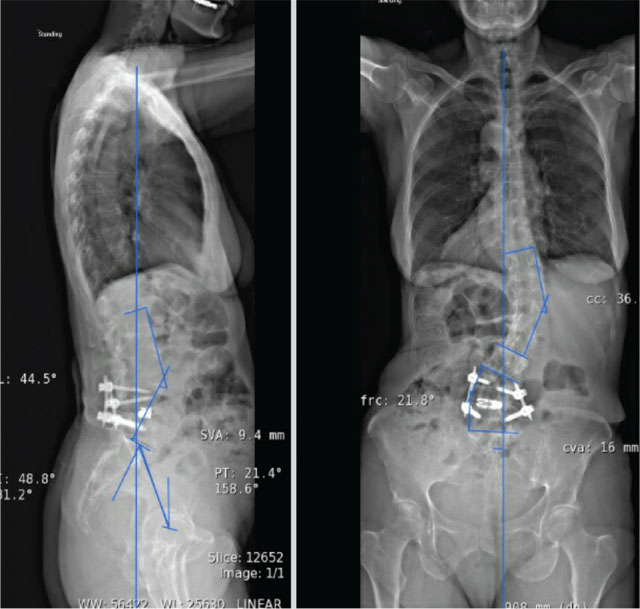
Pre- (A) and post- (B) operative radiographs demonstrating final reconstruction of adult degenerative spinal deformity.
Photo A:
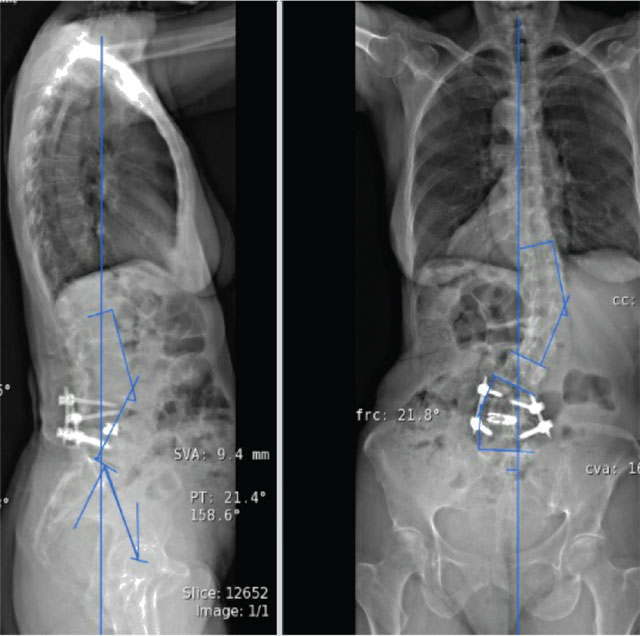
Photo B:

The prone transpsoas approach
The prone transpsoas approach is a novel one used for lateral lumbar interbody fusion that harnesses the advantages of minimally invasive surgery, such as requiring less cutting of soft tissue and smaller incisions, along with combined anterior and posterior access to the lumbar spine in a single position.
Traditionally, patients who undergo a lateral lumbar interbody fusion are positioned on their side, which allows placing an interbody cage between vertebral bodies and helps restore height or curvature to the spine. Following placement of the implant, patients are flipped to a prone position where neurosurgeons make an additional posterior incision to insert pedicle screws that hold the cage in place.
While the traditional two-stage, minimally invasive approach is the standard for spinal fusion surgery, moving the patient from the side to the prone position, including draping and undraping, can take anywhere from 30 to 90 minutes. If patients are overweight, this presents an additional challenge for hospital staff who need to rotate patients while they are still under anesthesia. The prone transpsoas technique obviates the need for positioning changes but is technically demanding for the surgeon given the ergonomics and visualization down the minimally invasive retractor with the patient in the prone position.
The benefits that Excelsius provides
Excelsius helps Rush surgeons during this procedure by providing three-dimensional, image- guided navigation, giving them improved accuracy for access to the lumbar intervertebral discs and, ultimately, placing the implant and screws. The navigation also helps surgeons adjust the implant’s position, if necessary, without having to reposition the patient. Moreover, using the traditional approach, surgeons have to rely on fluoroscopic imaging to ensure accurate implant placement. Excelsius’ intraoperative image guidance through robotic arms reduces the amount of radiation that operating room staff typically receive.

Correcting idiopathic scoliosis
Surgery for idiopathic scoliosis both corrects the curvature of the spine and, if possible, prevents curve progression as patients develop into adulthood. Surgeons attach metal implants to the spine, which are then reinforced with a single or double rod.
Challenges for surgeons in performing these surgeries are related to the flexible, mobile spines of their pediatric patients. The trajectories of the curves of patients with scoliosis and scoliotic curves can be so severe that they make implant and screw placement challenging even for the most experienced surgeons. In addition, the smaller size of these patients’ bones, which warrants the use of smaller screws than in adult deformity cases, can make implant and screw pullout a risk during surgery.
The benefits that Excelsius provides
Given these challenges, Excelsius can aid neurosurgeons in accurately placing the implants and screws via intraoperative CT guidance, even in the most extreme cases.

