History
A female patient in her 60s complained of worsening back pain with increasing kyphoscoliosis for almost 20 years. She reported pain in her low back and mid-back into her left shoulder blade region, which she rated a 5 out of 10 in intensity but worsens when she is upright. She also reported an increase in the size of the scoliosis prominence of her back.
She had increased pain with standing and walking, prolonged sitting or increased movements including twisting and turning while sleeping. Additionally, she noted stiffness and overall weakness because of this condition. When standing upright or walking, she could not hold herself upright and was bent forward. She was mostly concerned that her spinal deformity would worsen, and she would become a “crippled old woman”.
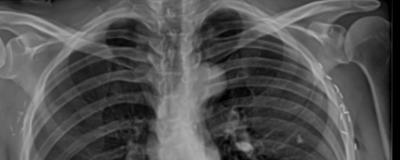
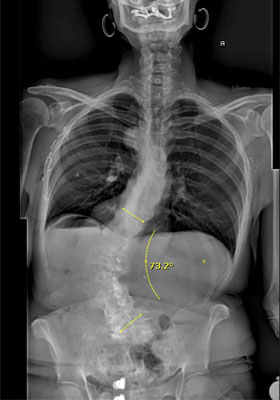
Presentation and Examination
A physical examination showed a significant left lumbar kyphoscoliosis with obvious prominence of the spinal curve on forward bending. She could bend forward approximately 80 degrees and could extend approximately 20 degrees at her hips.
Radiography showed that the patient had a left lumbar scoliosis that measured 73 degrees and had a sagittal imbalance of 18cm (forward leaning posture). Based on her prior scans her spinal deformity had progressed over the past few years.
Impression
The patient had increasing kyphoscoliosis on the thoracolumbar spine due to severe multilevel lumbar and thoracolumbar disc degeneration with resulting spinal instability, thoracolumbar kyphoscoliosis and global sagittal imbalance.
As a result, a major spinal reconstruction was recommended from T3 to her pelvis to hold her upright.

Treatment
These are long surgical procedures, so the surgery is planned in stages, starting with the lumbosacral/pelvic region and then, later in the day, extending the incision to instrument the thoracic region. Once the lumbosacral spine is exposed, spinal screws are placed within the vertebrae and into the pelvis bilaterally. This provides us with a strong base to perform the correction of the kyphoscoliosis above.
We then performed multiple posterior spinal osteotomies (Smith-Peterson osteotomies) across the apex of the kyphoscoliosis. This is done using a combination of burring and Kerrison rongeurs removing the posterior elements for the osteotomy, which resects the inferior and superior articular facets and the ligamentum flavum in a chevron pattern at each level to provide mobility across the deformity levels.
Once the osteotomies were completed, two 6.0 titanium rods are introduced into the pedicle screws to pull the spine into a proper alignment. This is done with cantilever de-rotational forces to close down the osteotomy site and correct the spinal deformity. A third rod is used at the lumbar spine for added support at the base of the spinal construct. The entire 15-vertebrae spinal fusion is then decorticated with a burr to stimulate the bone fusion process and bone graft is added to the decorticated spine. The long spinal incision is closed in layers over the rods.
Outcome
Three months following surgery, the patient reported only mild low-back pain, but was otherwise doing very well. She also gained back three inches of her height. She was amazed at her posture and anyone who saw her commented on how upright she was able to stand. Gradually she was able to increase the time and distance she was able to walk, doing so with normal gait and good posture.
Four years after the surgery, the patient is still doing great and has good posture and gait.


Analysis
Major surgical cases, such as this one, can take 8-12 hours of surgery and require a patient spend a week in the hospital post-operatively, plus an additional week in the rehab center. Complication rates can potentially be high, which would entail the need of additional surgeries. Before undertaking a major surgical correction, the patient needs to have good bone density and their age, along with their medical, surgical, and emotional status, should be considered as well.
Older patients have a ‘window of opportunity’ when their condition is appropriate to consider surgery and when they are too deconditioned or in poor medical condition to undergo such surgery. However, if an ideal patient is identified and their complications are appropriately managed, they report a high degree of satisfaction in being able to stand upright again.