Introduction
According to the American Cancer Society, colorectal cancer is the third most common cancer diagnosed in both men and women in the United States. The ACS estimates that approximately 107,000 new cases of colon cancer and 47,000 new cases of rectal cancer will be diagnosed in 2024. The incidence of colorectal cancers, according to the ACS, is roughly 1 in 23 for men and 1 in 25 for women; these rates can be influenced by individual patients’ risk factors, such as poor diet and obesity.
To reduce the risk of dying from colorectal cancer, screening by various methods has been implemented as a routine part of healthcare maintenance in the United States. Both noninvasive, stool-based tests and direct evaluation of the colon through colonoscopy have a robust body of evidence affirming the utility of these tests in saving lives.
Colonoscopy, in particular, is not only the gold standard for screening, but it can also detect precancerous polyps called adenomas. Therefore, it is the preferred method for colorectal cancer screening as it also has the unique potential for preventing cancer by detecting and resecting precancerous lesions. While most polyps will never turn into cancer, the vast majority of colorectal cancers come from polyps — in particular, adenomatous polyps. Over time, endoscopic imaging techniques, such as wide-angle lenses, several types of virtual chromoendoscopy, and various prosthetics for pleating colon have been introduced to improve the quality of colonoscopy by better detecting small, easy-to-miss colonic polyps.
The purpose of evolving, secondary technologies is to improve the adenoma detection rate (ADR). The ADR is calculated as a percentage of patients undergoing colonoscopy for screening who are found to have adenomas. A well-established benchmark for a given population sets the ADR at roughly 25%. ADR is arguably the single most important quality measure for colonoscopies as it has also been found that higher ADRs are correlated with lower rates of interval cancers. Thus, early detection and removal of adenomas is of supreme importance.
GI clinicians who perform colonoscopies with an ADR of <11% are most likely to have patients who develop interval colorectal cancer, that is, a cancer that develops within the surveillance interval. Providers with an ADR >43% see the lowest rates of colorectal cancer in their patients.
For example, if a patient is recommended to return to have another colonoscopy in 10 years and develops a cancer in eight years, that is an interval cancer. Whereas, if a patient is recommended to return to have another colonoscopy in three years and develops a cancer in 8 years, that is not an interval cancer. The interval recommended is based on the number and size of polyps, adequacy of bowel prep, family history, and possibly other subjective measures that affect visibility within the exam.
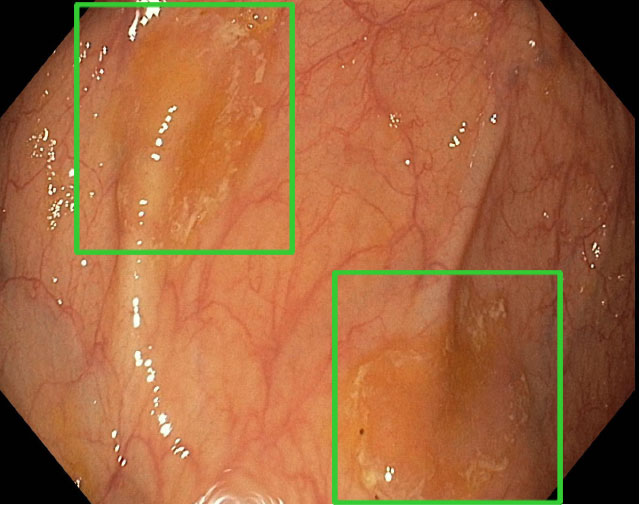
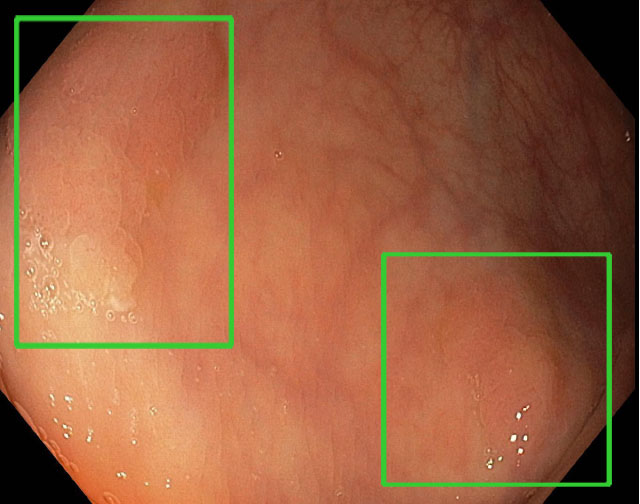
To improve ADR, RUSH has incorporated the use of a new artificial intelligence-based device, GI Genius, in nearly every endoscopy suite. With a flip of a button, it can be turned on as soon as the colonoscopy starts to help detect hard-to-see polyps. When a potential polyp is detected, a green box appears on the screen directing the endoscopist's attention to it.
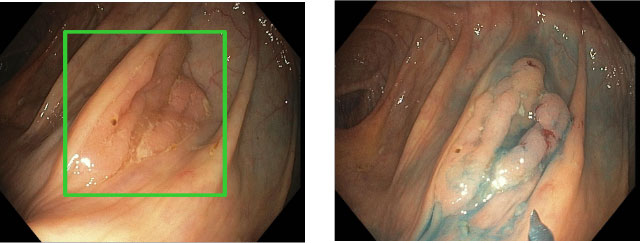
Examples of enhanced polyp detection
GI identifies and frames adenomas with a green box. The images in blue show what the polyp looks like after a dye is injected during the colonoscopy.


Conclusion
There is significant variability in how well endoscopists detect adenomas using existing technology. For physicians who have an inadequate ADR, the use of technology like GI Genius can certainly improve detection. Even for physicians who already meet this benchmark, GI Genius will further optimize their practice, as it has been shown to increase the ADR significantly even among experienced physicians with already robust detection rates. In this study, the use of artificial intelligence conferred a significant increase of the ADR between both “non-expert” (32.1% to 37.5%, p=0.023) and “expert” endoscopists (from 32.8% to 42.3% (p<0.001).
Even for physicians who have high ADRs, such as those at RUSH, the use of GI Genius will be able to increase detection rates of adenomas when compared to human operators alone. RUSH’s ADR has consistently been high: 10 years ago, our ADR was 38% and our current rate is 43%. Given each 1% increase in ADR decreases the risk of interval cancer by 3%, however, we can improve our ADR, which ultimately translates into clinically relevant outcomes for our patients. In order to continue to enhance the quality of patient care, RUSH became the first academic medical center in Illinois to use artificial intelligence to further that goal.

