History
A female patient in her 50s was diagnosed with stage IV colon cancer with metastases in her rectum. Her primary colon tumor is rectosigmoid and located 12 cm from the anal canal. She also had adenocarcinoma of the rectum.
She also had a good response after 10 cycles of FOLFOX and Mvasi. The patient was on maintenance therapy of 5-FU and Leucovorin and Mvasi.
Presentation and Examination
The patient responded well to chemotherapy; in a six-month period from December 2021 to May 2022, there was a significant interval decrease in the size of multiple hepatic metastatic lesions. The patient had approximately 22 peripherally enhancing liver metastases.
Our main concern is that the patient has received more than six cycles of chemotherapy, which may have negatively affected liver quality and regenerative capacity. The risk of recurrence is also increased due to the presence of preexisting and now disappeared lesions. However, recurrence with more than 10 metastases is universal, as is the potential for lung metastases in the future.
We believe the patient would be an excellent candidate for portal vein / hepatic vein embolization (PVE/HVE or double vein embolization) as part of the international DRAGON trial. We advised her oncologist to discontinue the maintenance chemotherapy in September 2022, then scheduled the two-stage hepatectomy for October.
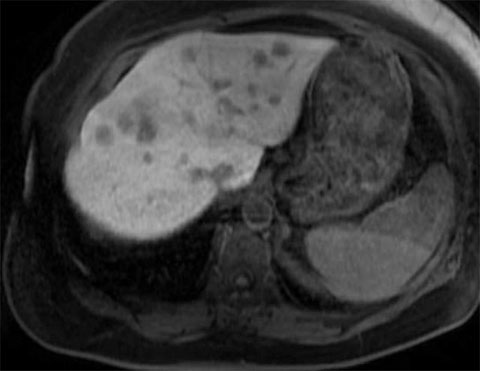
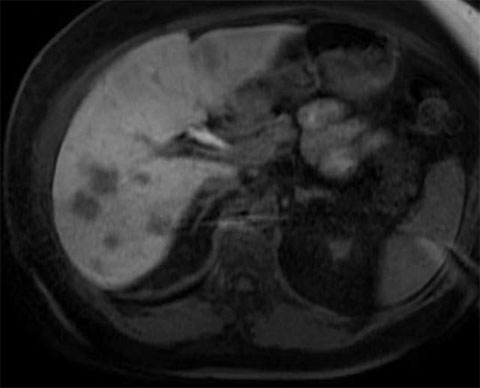
Pre-treatment MRIs

Treatment
Stage 1: Cleaning of the left hemiliver
We identified 12 total lesions on the patient’s liver; five of these were in segment 2, one was in segment 1, four were in segment 3 and two were in segment 4A.
In the following order, we used microwave ablation the following lesions: lesions 10 on the middle hepatic vein, lesion 9 in segment 4B, lesion 3 in segment 2, lesions 2 and 5 in segment 3, then lesion 4.
We then proceeded with resection of the following lesions in this order: partial hepatectomy of lesion complex 8, partial hepatectomy of lesions 6 and 7, and a wedge resection lesion 11. When we encountered the caudate lesion, it was superficial and would be too difficult to retract; instead, we performed an ablation on it instead.
Targeting this many lesions on one side of the liver is highly difficult that requires two attending surgeons to be successful.
All of the lesions showed signs of extensive regression from chemotherapy.
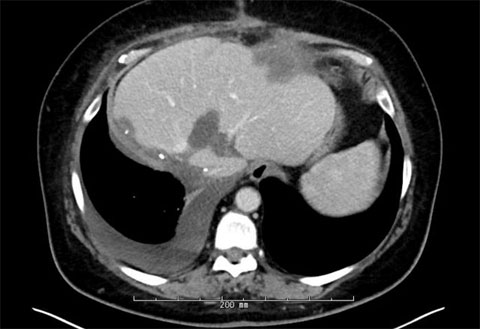
Post-first-surgery MRIs



Stage 2: Right hepatectomy
The patient had a successful percutaneous embolization of the right portal vein and transjugular embolization of the right hepatic vein.
Four weeks later, the patient came in for the second stage of the procedure, the right hepatectomy.
The patient had adequate growth in the liver remnant and was brought back for the removal of the right lobe of her liver where we removed approximately 70% of her liver, leaving 30% of it behind.
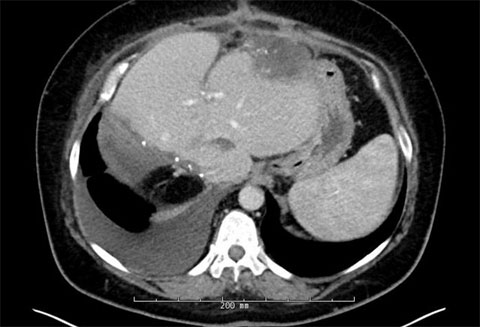
Post-second-surgery MRIs

Outcome
The patient is doing very well and recovered very nicely from her liver surgeries. Currently, the patient is getting radiation to her rectal cancer and will then undergo resection of the primary tumor.
Analysis
Resection of colorectal liver metastases (CLRM) is potentially curative when used a multidisciplinary treatment team. This patient, who had numerous liver metastases across both sides of her liver, was initially told her tumors were unresectable. But after chemotherapy and careful planning of her liver surgery, we were able to treat all of her liver disease.
Yet, despite the evidence supporting liver resection for patients with CRLM, access to liver resection is still not universal in this patient group. Between 1991 and 2001, only 6% of patients with CRLM underwent liver resection.(1) This has since risen to the current rate of approximately 15%.(2)
Given that approximately 30% of patients with CRLM are estimated to benefit from liver resection(3), this means that up to half of patients who would benefit from liver resection are not sent for evaluation for liver resection. This represents significant underutilization of liver resection for CRLM and many patients with this disease, who are told they are unresectable, are, in fact, resectable when assessed by a liver surgeon.
Every patient with liver metastases from CLRM should be sent for consultation with a hepatopancreatobiliary surgeon before they are told they are unresectable.
Sources
- Cancer. 2007; 109(4):718-726.
- Cancer. 2020;126(2):281-292.
- JAMA Surg. 2020 Oct 1;155(10):909-910.

