Given its rarity, scapular chondrosarcoma does not have a well-defined treatment protocol, and traditional reconstructive techniques with standard prosthetic options often result in profound functional limitations for patients. Patients with high functional and occupational demands may benefit from a novel reconstructive approach using custom, 3D-printed implants. In the first case of its kind in Chicago, a multidisciplinary team of Rush surgeons reconstructed the shoulder of a 49-year-old female hairdresser with low-grade chondrosarcoma using a patient-specific, 3D-printed implant.
Custom 3D-Printed Scapular Implant for Functional Reconstruction Following En Bloc Resection of Low-Grade Chondrosarcoma
A Case Report By John Streepy, MS, Zachary Butler, BS, Xavier Simcock, MD, and Alan T. Blank, MD, MS
Introduction
Chondrosarcoma is the second most common primary malignant bone tumor, accounting for approximately 20% of all primary bone malignancies.[1] Chondrosarcoma most frequently arises in the pelvis, femur, and humerus,[2] and involvement of the scapula is rare, presenting unique surgical and functional challenges. Given the scapula’s role in shoulder stability and shoulder motion, tumor resection in this region can significantly impact a patient’s function and quality of life.
Surgical management of scapular chondrosarcoma typically involves surgical resection. Low-grade chondrosarcoma may be treated with intra-lesional curettage and adjuvant treatment, while higher-grade lesions are treated with en bloc resection to achieve negative margins and minimize the risk of local recurrence.[3,4] Due to the scapula’s complex anatomy and the goal of preserving shoulder function, reconstruction strategies must be carefully considered. Resection of significant portions of the scapula, particularly those that include the glenoid, leave patients with essentially a flail shoulder with limited to no function. When considering reconstruction options, the surgical team should consider prosthetic reconstruction, biological techniques such as allograft or autograft reconstruction, or leaving the patient with a flail shoulder.[3] Recent advancements in 3D printing technology have enabled the creation of patient-specific implants potentially allowing for anatomic restoration and improved functional outcomes in these situations.[5]
This report presents the case of a 49-year-old female diagnosed with low-grade chondrosarcoma of the left scapula including the entirety of the glenoid and three quarters of the body of the scapula. Given her occupational demands as a hair stylist, she would benefit from significant shoulder function postoperatively. Thus, she underwent en bloc resection with complex scapular reconstruction using a custom 3D-printed implant and shoulder arthroplasty. This case highlights the multidisciplinary approach required for optimizing oncologic control while preserving upper extremity function.
Case report
A 49-year-old female presented with intermittent left shoulder pain for numerous years, which she attributed to a fall years ago. This pain worsened over the last year, prompting evaluation by a non-operative sports medicine physician. Initial radiographs revealed an incidental mass in the left scapula and shoulder joint, leading to further workup. The patient denied constitutional symptoms such as weight loss, night sweats, or fever. She also denied numbness, tingling, or pain at rest, reporting discomfort primarily with active shoulder motion and palpation over the affected area. Her medical, surgical, and family histories were unremarkable. She was never a smoker. She worked as a hairdresser, and her limited shoulder function was negatively affecting her ability to work.
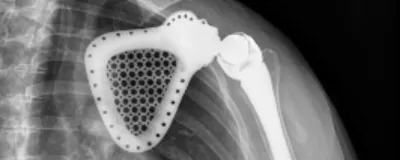
On physical examination, the patient’s left shoulder abduction was 45 degrees, limited by pain. Forward flexion was 90 degrees, limited by pain. Internal rotation on the left was to about the L5 spinal level, limited by pain. She also had pain with the drop arm test on left. Radiographs as well as advanced imaging revealed a well-demarcated lesion involving the scapula with no evidence of cortical destruction or soft tissue invasion (Figure 1).
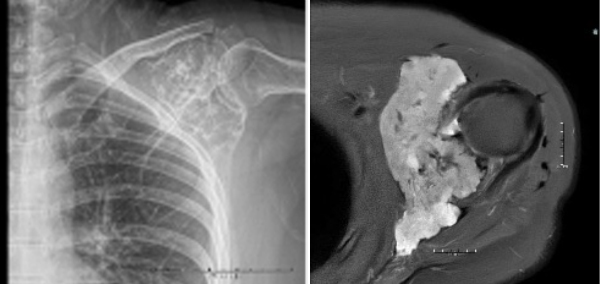
The decision to proceed with core needle biopsy was made, which demonstrated a low-grade chondroid lesion. The case was discussed at multidisciplinary tumor board, where surgical management was recommended given the lesion’s location and the patient's occupational necessity for shoulder function.
The surgical team recommended en bloc resection of the scapula with complex reconstruction utilizing a custom 3D-printed scapular implant and reverse total shoulder arthroplasty. The patient was counseled on the risks and benefits of reconstruction versus a flail shoulder approach and elected to proceed with reconstruction to optimize functional outcomes.
The patient underwent en bloc resection of the left scapula with complex reconstruction. Intraoperatively, a longitudinal incision was made extending from the inferior scapula toward the supraclavicular region. Muscular attachments were carefully dissected to preserve as much functional tissue as possible while achieving oncologic control. The scapula was circumferentially mobilized, with careful dissection around the neurovascular structures, including the axillary nerve. Given the tumor's proximity to the acromioclavicular joint, the clavicle was osteotomized a few centimeters medial to the joint. The scapula was removed en bloc, and hemostasis was achieved. The surgical field was irrigated, and a sterile re-draping was performed before proceeding with reconstruction.
Reconstruction was performed using a patient-specific, 3D-printed scapular implant (Onkos) with an ExacTech captured shoulder arthroplasty system. The implant was secured in place, and soft tissue balancing was optimized to facilitate postoperative mobility. A drain was placed, and the wound was closed in a layered fashion. The patient tolerated the procedure well with no immediate complications.
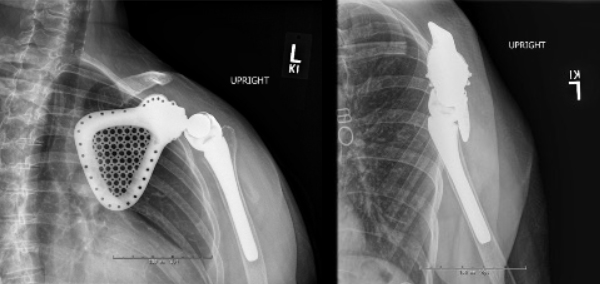
Postoperatively, the patient was admitted for pain management, perioperative antibiotics, DVT prophylaxis, and initiation of physical therapy. She was placed in a shoulder immobilizer and maintained non-weightbearing on the left upper extremity. Histopathologic examination of the resected specimen confirmed low-grade chondrosarcoma with negative surgical margins. At her five-month follow up, she is out of her sling the majority of time and works with physical therapy two times a week. She continues to improve with both passive and active range of motion of the shoulder but endorses a pinching sensation over the anterior and posterior shoulder as well as intermittent numbness to the lateral aspect of the upper arm.
Discussion
Chondrosarcoma of the scapula is a rare malignant bone tumor, comprising a fraction of all chondrosarcoma cases. The scapula's complex anatomical relationships with critical neurovascular structures pose significant challenges in both tumor resection and reconstruction. The axillary nerve, suprascapular nerve, and brachial plexus must be carefully dissected and preserved to prevent significant functional deficits. Additionally, the subclavian and axillary vessels course near the scapula, requiring surgical planning to achieve complete tumor resection while minimizing the risk of vascular injury and excessive blood loss. Unlike other long bone malignancies, which may allow for standard segmental resection with endoprosthetic replacement or allograft reconstruction, scapular tumors require a more nuanced approach due to the bone’s integral role in upper extremity kinematics and the lack of widely available reconstructive options.
Due to its rarity, scapular chondrosarcoma does not have a well-defined standardized treatment algorithm. As with other chondrosarcomas, surgical resection remains the primary treatment, as these tumors are largely resistant to chemotherapy and radiotherapy.[6] The primary goal of surgery is to achieve negative margins to reduce the risk of local recurrence, which can be challenging given the scapula’s complex anatomy. In many cases, a more conservative approach, such as intralesional curettage or marginal excision, is considered sufficient to balance oncologic control with functional preservation. Wide excision with full prosthetic replacement is not typically performed for low-grade lesions; however, due to the size and destructive nature of this tumor, an intralesional procedure would not have been possible. Additionally, given the patient’s profession and high functional demands, long-term mobility and upper extremity function were prioritized. This led to the decision for a more extensive surgical approach, including en bloc resection and custom 3D-printed scapular reconstruction. This case underscores the importance of incorporating patient goals and functional needs into surgical decision-making, highlighting that tumor staging alone should not dictate the extent of surgical intervention.
The use of 3D-printed scapular implants in oncologic reconstruction remains exceedingly rare, with limited cases reported in the literature.[5] Historically, reconstruction following scapulectomy has been performed using allografts, autografts, or flail shoulder techniques.[3] However, these methods may result in compromised function, particularly in patients requiring maximal shoulder range of motion. The advent of patient-specific 3D-printed implants provides a novel approach that potentially allows for anatomical restoration of the scapula while integrating shoulder arthroplasty components for potential improved biomechanics. While long-term data on the durability and functional outcomes of these implants remain limited, early reports suggest promising results in restoring shoulder mobility and reducing postoperative complications related to soft tissue imbalance.[5]
In this case, the decision to proceed with a custom scapular implant was guided by the patient’s strong desire to maintain functional shoulder mobility. As a hairdresser, the ability to abduct and forward elevate the shoulder is essential for her profession. Traditional comprehensive reconstructive approaches, including muscle flap techniques without bony reconstruction, would likely have resulted in profound functional limitations. The custom 3D-printed scapular implant offered the best opportunity to restore a functional glenohumeral articulation, optimizing both stability and range of motion. While the long-term success of this approach remains to be determined, this case represents a significant advancement in functional limb-salvage surgery for scapular malignancies.
Looking ahead, continued research and long-term follow-up will be necessary to assess implant durability, functional outcomes, and the risk of complications such as implant loosening or wear. This case underscores the importance of a multidisciplinary approach, incorporating tumor biology, biomechanics, and patient-specific functional goals to optimize oncologic and reconstructive outcomes.
Conclusion
In summary, we describe the case of a 49-year-old female with low-grade chondrosarcoma of the left scapula, treated with en bloc resection and reconstruction using a custom, 3D-printed scapular prosthesis and reverse total shoulder arthroplasty. The complex case — the first of its kind in Chicago — highlights the importance of advanced preoperative planning, multidisciplinary collaboration, and patient-specific implant technology.
Clinical message
Chondrosarcomas of the scapula are rare and pose significant surgical challenges due to their involvement of the shoulder joints’ functional motor units, as well as potential surrounding neurovascular structures. Additionally, postoperative function in these patients historically has been very limited. For high-demand patients, reconstruction may optimize oncologic control while preserving function. As more long-term data is needed on the durability of 3D-printed implants, Rush will continue to collaborate with other institutions to evaluate outcomes in this and other patient populations.
Learning point of the article
This case highlights the evolving role of 3D printing in orthopedic oncology. The ability to create patient-specific implants tailored to an individual’s anatomy represents a paradigm shift in complex reconstructions, particularly in rare oncologic cases where standard prosthetic options are less optimal.
References
- Murphey MD, Walker EA, Wilson AJ, Kransdorf MJ, Temple HT, Gannon FH. From the archives of the AFIP: imaging of primary chondrosarcoma: radiologic-pathologic correlation. Radiographics. 2003 Sep-Oct;23(5):1245-78.
- Thorkildsen J, Taksdal I, Bjerkehagen B, et al. Chondrosarcoma in Norway 1990-2013; an epidemiological and prognostic observational study of a complete national cohort. Acta Oncol. 2019 Mar;58(3):273-82.
- Biazzo A, De Paolis M, Donati DM. Scapular reconstructions after resection for bone tumors: a single-institution experience and review of the literature. Acta Biomed. 2018 Oct 8;89(3):415-22.
- Leerapun T, Hugate RR, Inwards CY, Scully SP, Sim FH. Surgical management of conventional grade I chondrosarcoma of long bones. Clin Orthop Relat Res. 2007 Oct;463:166-72.
- Grossi S, D'Arienzo A, Sacchetti F, et al. One-step reconstruction with custom-made 3D-printed scapular prosthesis after partial or total scapulectomy. Surg Technol Int. 2020 May 28;36:341-6.
- Gelderblom H, Hogendoorn PC, Dijkstra SD, van Rijswijk CS, Krol AD, Taminiau AH, Bovée JV. The clinical approach towards chondrosarcoma. Oncologist. 2008 Mar;13(3):320-9.

