Introduction
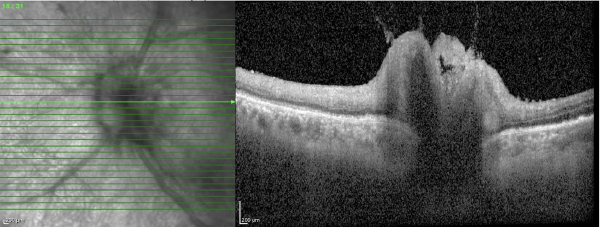
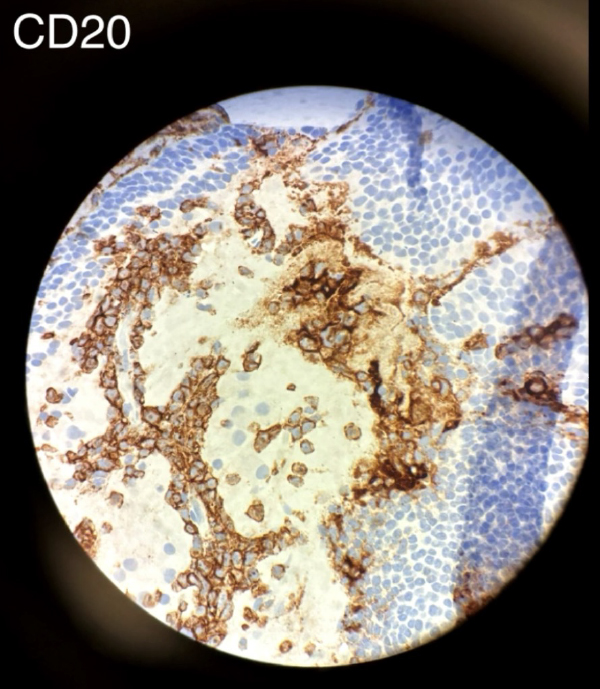
Lymphomatous optic neuropathy (LON) is a rare but vision-threatening manifestation of central nervous system (CNS) lymphoma, characterized by the direct infiltration of malignant cells into the optic nerve. It can occur as a primary process or, more commonly, as a secondary spread from systemic non-Hodgkin’s lymphoma, such as diffuse large B-cell lymphoma (DLBCL). Early diagnosis is critical to preserving vision and life, yet detection remains a significant clinical challenge.
Current clinical guidelines for the diagnosis of vitreoretinal and optic nerve lymphoma heavily rely on neuro-imaging and cerebrospinal fluid (CSF) analysis. However, classical CNS surveillance modalities, including magnetic resonance imaging (MRI) and standard lumbar puncture cytology, are not always reliable in detecting early or isolated infiltration. In the absence of definitive findings on standard workup, clinicians face a dilemma regarding the timing and necessity of invasive procedures.
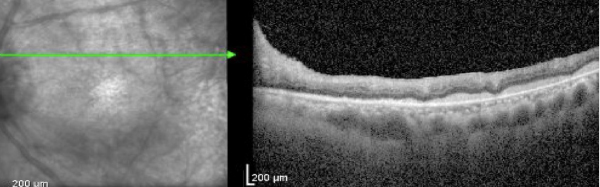
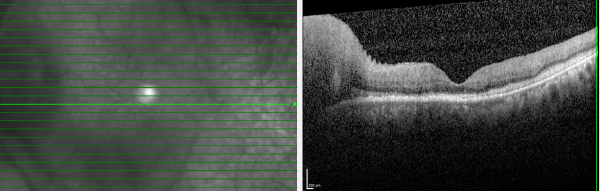
This case report discusses a patient with a history of DLBCL who presented with progressive optic neuropathy despite negative neuro-imaging and cerebrospinal fluid analysis. The case illustrates the limitations of standard CNS surveillance in detecting occult infiltration and highlights the necessity of tissue biopsy for definitive diagnosis.